Proton density oblique coronal MR image in 41 year old male patient with trauma showing focal fracture in the greater tuberosity of the humerus (arrow head) with full thickness tear in the supraspinatus tendon and retraction of the tendon fibers (arrow) suggestive of full thickness avulsion tear.
T1 TSE oblique coronal MR image showing focal fracture in the greater tuberosity of the humerus (arrow head) with absent hypointense supraspinatus tendon.
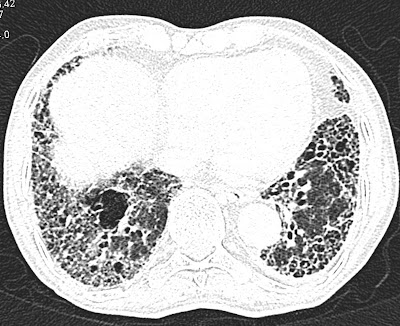
Axial T2 Medic (GRE) image showing fracture and tendon tear.
Sagittal STIR image showing full thickness tear and absent tendon fibers.
Discussion:
- Full-thickness avulsion tears of the tendon away from the greater tuberosity are less common.
- Massive tears often extend posteriorly to involve the infraspinatus tendon or extend anterior to tear, the anterior interval and subscapularis tendon.
- If an acute complete supraspinatus tendon tear is identified, surgery is often scheduled within the next several days so that the tendon can be repaired before the development of retraction or atrophy.
- Angled oblique sagittal T2/STIR images perpendicular to the plane of the supraspinatus tendon can better delineate the partial and full thickness tears.