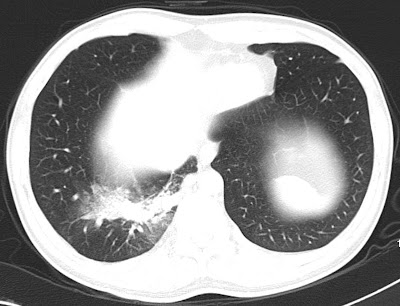
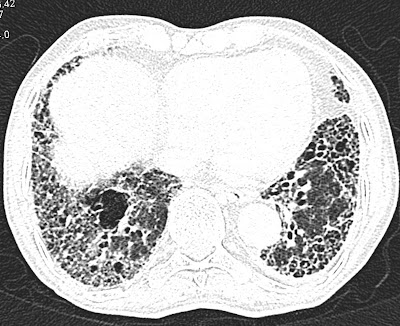
CT scan axial section in a 28 Year old female with pain abdomen since 2 years showing well defined predominantly fat density round mass lesion seen in the pelvis in the mid line and towards right side with areas of calcification (Rokintasky protruberence), soft tissue and fluid components in the dependent part. Features are consistent with dermoid.
Discussion:
A term dermoid is used now a days instead of teratomas which derived from more than one germ layer.
The contents of the dermoid include hair, teeth, fat, skin, muscle, endocrine tissue and ectodermal tissue predominates among these.
- Mature cystic teratomas are commonly referred as dermoid cysts.
- They are most common ovarian neoplasm.
- Mature cystic teratomas of the ovary is invariably benign. Rarely (1-3%) my undergo malignant. Prognosis is poor for such tumors.
Age: Can occur at any age. More common during reproductive age (16-55) and peak at 20-40. 50% of adnexal neoplasms are dermoid during adolescence.
Location: Most commonly ovary, bilateral in 8-25%.
Other locations: Mediastinum, retroperitoneum, cervical region, brain
Clinical findings: Frequently incidentally detected.
- Abdominal pain as in our patient.
- Mass
- Abnormal uterine bleeding.
- Back pain.
- Bladder and GI symptoms.
Imaging findings:
Radiograph:
- A soft tissue mass if it is large.
- A fat containing mass of fat density - the density of mass is lower than surrounding tissues.
- Characteristic calcification -Pop cord calcification or rim like or tooth or other bone (clavicle).
Ultrasonography:
- It has been reported as 98% of positive predictive value for ovarian dermoids.
- Compled mass with echogenic components.
- Mass is echogenic most of the times and producing "dirty acoustic shadowing"
- It may be purely cystic in 9-15% or purely solid in 10-31% cases.
CT scan:
- It demonstrates mass having fat, fluid and calcification (Tooth) as its contents.
- Rim like calcification, Tooth or other bone (clavicle) -Rokintasky protruberence.
- Fat-fluid levels may be seen.
MRI:
- The lesion shows hyperintense fat on T1 with hypointense fluid.
- Hyperintense on T2.
- Fat appears hypointense (suppressed) on STIR or T2 fat sat images.
Treatment:
- Surgical removal - May have risk of chemical peritonitis if ruptured.
Complications:
- Torsion.
- Rupture.
- Infection.
- Autoimmune hemolytic anemia - very rare.
Differential diagnosis:
- Benign or malignant ovarian tumor.
- Endometrioma.
- TO Abscess.
- Pedunculated uterine fibroid.
- Hydrosalpinx.
- Ectopic kidney.
- Pelvic kidney.