60 Year old female with history of pain abdomen and weight loss. USG showing well defined hypoechoic mass lesion in the region of body and tail of the pancreas with mild to moderate vascularity. It also shows few necrotic areas.
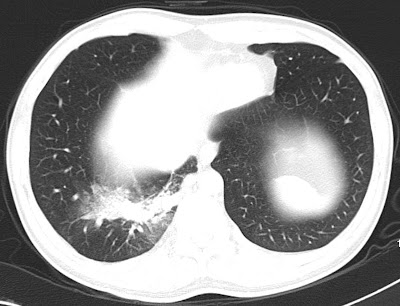
Axial CT scan showing well defined heterogeneously enhancing mass lesion arising from the body and tail of the pancreas showing areas of necrosis and causing mass effect on the adjacent structures however no obvious infiltration of the surrounding structures.
USG Guided FNAC showing the lesion with echogenic linier needle (arrow head)
Discussion:
Pancreatic adenocarcinoma is the second most common cause of death from GI cancers.
Adenocarcinoma ususally arise from pancreatic ducts (99%) and other site being acinar cells (1%).
More than 90% of pancreatic cancers appear in the late stage of disease.
Role of radiology:
1. Early detection.
2. Determination of resectability of the tumor.
3. Relationship to surrounding vasculature.
Multiphasic contrast enhanced study of upper abdomen in Multislice CT scan is the preferred investigation of choice.
CT Scan features include:
1. Alterations in morphology of the gland.
2. Obliteration of peripancreatic fat.
3. Loss of sharp margins with surrounding structures.
4. Involvement of adjacent vessels - is the sign of unresectability.
5. Regional lymph node enlargement.
5. Pancreatic ductal dilatation, pancreatic atrophy, and obstruction of the common bile duct (CBD)
MRI: Role of MRI is yet to be firmly established. T1-weighted fat-suppressed spin-echo and single–breath-hold gradient-echo fast low-angle shot (FLASH) sequences with gadolinium enhancement are valuable for tumor detection.
USG:
The lesion may have a variable appearance on US. It may be hypoechoic, isoechoic, or hyperechoic to the normal pancreas.
Pancreatic ductal dilatation and biliary ductal dilatation are easily demonstrated in patients with a tumor in the head of pancreas that causes an obstruction.
Lymphadenopathy, the relation of the tumor to peripancreatic vessels, and the tumor margins are demonstrated less reliably with US than with other modalities.
More than 90% of pancreatic cancers appear in the late stage of disease.
Role of radiology:
1. Early detection.
2. Determination of resectability of the tumor.
3. Relationship to surrounding vasculature.
Multiphasic contrast enhanced study of upper abdomen in Multislice CT scan is the preferred investigation of choice.
CT Scan features include:
1. Alterations in morphology of the gland.
2. Obliteration of peripancreatic fat.
3. Loss of sharp margins with surrounding structures.
4. Involvement of adjacent vessels - is the sign of unresectability.
5. Regional lymph node enlargement.
5. Pancreatic ductal dilatation, pancreatic atrophy, and obstruction of the common bile duct (CBD)
MRI: Role of MRI is yet to be firmly established. T1-weighted fat-suppressed spin-echo and single–breath-hold gradient-echo fast low-angle shot (FLASH) sequences with gadolinium enhancement are valuable for tumor detection.
USG:
The lesion may have a variable appearance on US. It may be hypoechoic, isoechoic, or hyperechoic to the normal pancreas.
Pancreatic ductal dilatation and biliary ductal dilatation are easily demonstrated in patients with a tumor in the head of pancreas that causes an obstruction.
Lymphadenopathy, the relation of the tumor to peripancreatic vessels, and the tumor margins are demonstrated less reliably with US than with other modalities.