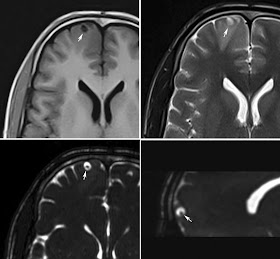
MRI Brain of 26 year old male presented with seizures, T1 image showing well defined small hypointense lesion in the right frontal cortical region, which is showing hyperintense on T2 image. CISS 3D - heavily weighted T2 images (bottom row) showing fluid intensity lesion with small hypointense focus. The findings are consistent with neurocysticercosis.
This Blog contains practically relevant interesting cases with relevant references, links and images.
Monday, January 31, 2011
Syrinx - MRI
Cervical spine MRI in a 54 year old male patient showing focal dilatation of the central spinal canal with no enhancing focal lesion within the cord. The features are consistent with the focal syrinx.
Discussion:
Hydromyelia: An accumulation of cerebrospinal fluid (CSF) may lead to simple distention of the central canal of the spinal cord lined by ependymal cells.
Syringomyelia: an accumulation of CSF may dissect into the surrounding white matter to form a paracentral cavity, which is not lined by ependyma.
syringohydromyelia: Combination of both which is seen in most of the cases.
I - In 1973, Barnett et al classified syringohydromyelic cavities into 5 types:
- Communicating (with the subarachnoid space, usually at the level of the obex at the inferior aspect of the fourth ventricle)
- Posttraumatic
- Tumor-related
- Arachnoiditis-related
- Idiopathic.
II - Milhorat et al, the intramedullary cavities were classified into communicating, noncommunicating, and atrophic types.
III - Noncommunicating syringes are subdivided into 6 types:
- Chiari II malformation with hydrocephalus
- Chiari I malformation without hydrocephalus
- Extramedullary compressive lesions at the craniocervical junction or along the length of the spinal canal
- Spinal cord trauma
- Intramedullary tumors and intraperimedullary infections
- Multiple sclerosis
Tuesday, January 25, 2011
Endometrioma - MRI
32 year old female underwent MRI for pain in the lower abdomen a) T2 weighted fat saturated axial image showing bilateral ovarian cysts and one of the cyst in the right ovary (arrow) shows hemosiderin fluid levels (T2 shading). b) The same cyst in the T1 WI showing hyperintese fluid with hypointense hemosiderin. The features are consistent with endometrioma.
Discussion:
Endometriosis is defined as the presence of endometrial glandular tissue outside of the uterus. Endometriomas are frequently present in the premenopausal stage. It is present in 32% of women with infertility and/or pelvic pain between the ages of 20 and 45 years. Incidence is 29 - 54%.
USG:
The spectrum of findings on transabdominal sonography (TAS) is wide due to difficulty in accurately characterising the lesion. On TVS, the endometrioma is seen as a round homogeneous hypoechoic 'tissue', of low-level echoes, with a clear demarcation from the parenchyma and without papillary proliferation is present in at least 80% of cases of endometriomas.
Endometrioma do not shows acoustic streaming where as other cysts shows the same. 'Acoustic streaming' is a useful tool for differentiating endometriomas from other benign cystic lesions. 'Acoustic streaming' is defined as the bulk movement of fluid due to a sound field caused by energy transfer from an US wave to a fluid. The presence of hyperechoic wall foci (punctate peripheral echogenic foci) on ultrasonographic examination is very specific to endometriomas.
The diagnostic points described for endometrioma by different authors as follows:
- A round-shaped homogeneous hypoechoic 'tissue' of low-level echoes without papillary proliferations associated with 'poor' vascularization (defined by Aleem et al. in 1995);
- A round-shaped homogeneous hypoechoic 'tissue' of low-level echoes with an echogenic portion in which no flow is detected (atypical findings).
MRI:
MRI demonstrates these endometriomas as cystic masses with very high signal intensity on T1-weighted images and very low signal intensity on T2-weighted images with layering of blood products termed as "T2 shading". Another common finding is a very dark peripheral rim (arrowhead), due to hemosiderin deposition, which is also the result of blood degradation.
Recently susceptibility-weighted imaging (SWI) has shown to contribute to the diagnosis of endometrioma by depicting hemosiderin deposition in the cyst wall.Thursday, January 13, 2011
HIV Encephalopathy - MRI
MRI axial fluid attenuation inversion recovery (FLAIR) images in 48 year old male with HIV showing generalised cerebral atrophy with diffuse white matter hyperintenisty signal change seen in the bilateral periventricular frontal and paroeto-occipital regions consistent with HIV encephalopathy.
Discussion:
Clinically it is usually presents with progressive dementia, initially cognitive impairment and later accompanied by motor symptoms like gait disturbance and tremor. Collectively this is called as AIDS dementia complex.
Histopathology may reveal subacute encephalitis, cerebral atrophy and demyelination.
CT - The sole finding in most of the patients may be cerebral atrophy. In progressive advanced patient may see periventricular confluent white matter hypodensities.
MRI- Cerebral atrophy, classical appearance of confluent, bilateral and symmetrical white matter lesions seen as diffuse white matter change in the periventricular regions and centrum semiovale, with relativesparing of the subcortical white matter and posterior fossa structures. These lesions shows hyperintense on T1 and iso to hypointense on T1 images. There will be no contrast enhancement or mass effect.
MR Spectroscopy shows decreased N Acetyl Aspartate and increased choline peaks and changes in the glutamate and glutamine levels.
Choledocholithiasis - MRCP
45 year old female with pain abdomen and jaundice underwent MRI and MRCP revealed calculus in the distal common bile duct obstructing the lumen resulting in mild to moderate upstream dilatation of the intra hepatic biliary radicals.
Discussion:
Choledocholithiasis is relatively common, seen in in 6 - 12% of patients who undergo cholecystectomy. They may present with biliary colic, ascending cholangitis, obstructive jaundice, acute pancreatitis. Stones within the bile duct may form either in situ or pass from the gallbladder, and when recurrent tend to be pigment stones, and are thought to be associated with bacterial infection.USG: Sensitivity varies from 13 to 55%. Features include dilated duct with stones visualized within. Recently endoscopic ultrasonography (EUS) has also been used with very high sensitivity and specificity.
CT: Moderate sensitivity of 65 - 88% but have to look for very subtle findings. They are
- Target sign - Central rounded density of stone with surrounding lower attenuating bile or mucosa.
- Rim sign: Stone is outlined by thin shell of density.
- Crescent sign: Bile eccentrically outlines luminal stone, creating a low attenuation crescent.
- Calcification of the stone: unfortunately only 20% of stones are of high density
MRCP: is the gold standard investigations for biliary lithiasis replacing the ERCP. Filling defects are seen within the biliary tree on thin cross-sectional T2 weighted imaging.
Tuesday, January 11, 2011
Carcinoma Prostate - PET/CT
63 year old male patient operated for carcinoma prostate came for FDG PET/CT evaluation for recurrent tumor. Coronal CT and the PET/CT fused image showing non FDG avid multiple sclerotic lesions in the sacrum and right iliac bones. Multiple similar lesions also were seen in various vertebral bodies, scapulae and ribs (not shows here)
Discussion:
PET/CT in combination with PSA levels can play a significant role in detecting and staging prostate cancer. Although Prostate-specific antigen measurements are considered a useful organ-specific marker, but they are alone not necessarily an adequate tumor marker.
Localized disease within the prostate and pelvic lymph nodes can be difficult to image with PET/CT because of the proximity of bladder activity as there is will be spillover of radiotracer uptake.
The radiotracers used in prostate PET/CT:
- Fluorodeoxyglucose (FDG): have a role in the detection of lymph node metastases, particularly in patients with relapsed disease after primary treatment. The sensitivity is around 50%. FDG-PET has an excellent detection rate for lytic skeletal metastases, but it has a poor detection rate for sclerotic metastases as in our case.
- Carbon 11 (C11)–acetate and C11-choline (18F-Choline): Shown promising alternative but they are less readily available and still under assessment. Few recent studies have showed conflicting results as one study says there is relative high rate of false-negative results as prostatic disorders other than cancer may accumulate 11C-choline. Some other study shows C11-choline PET/CT can differential prostate carcinoma from benign hyperplasia, chronic prostatitis, or normal prostate tissue. The C11 choline has shows promising results in staging of the tumor; however it still needs more studies.
To conclude sextant /10 core biopsy along with PSA are the mainstay of diagnosis and FDG PET/CT and C11 Choline PET/CT are for the staging, treatment planning and response evaluation.